Summary of the Ready to Eat study: Helping children progress from tube feeding to eating
Home-based behavioural interventions to help children progress from tube to oral feeding
The full article describing some of this research is at the link here: https://doi.org/10.1093/jpepsy/jsz014, and was awarded the Diane J. Willis Award for Outstanding Article. This shows the recognition of this work in having the potential for impact on the field of psychology.
Why is this research taking place?
Behavioural interventions (Applied Behaviour Analysis) have the strongest research evidence in the treatment of childhood feeding disorders, including tube weaning.
Treatment is usually conducted in specialized centres (like hospitals), but in Aotearoa we do not have access to these settings, and specific interventions for tube dependency are not yet funded.
Sometimes it is not clear whether children continue to make progress over the longer-term (like months after the intervention), and whether important nutritional progress occurred - like whether tube feeding stopped.
Who is involved?
Twelve children (aged 1-14 years) have received the intervention so far, who were dependent on nasogastric (NG) or gastrostomy (G) tubes. Most received all of their nutrition via the tube and refused to eat all foods. Children had various medical conditions (e.g., gastrointestinal conditions) and eight had a developmental disability.
A psychologist (Sarah Leadley) led mealtime sessions initially, with caregivers present and with the involvement of the child’s health professionals (paediatrician, dietitian, and speech language therapist).
What is done?
The process involves assessment, followed by an individualised intervention for the child. This usually takes place over an intensive period (2 weeks of consecutive days). Assessment involves a detailed interview about the child’s feeding. We ask families about situations where their child had eaten or even approached food; “ what type of food, how did you feed it, how much?” Some of these situations are then tested during meals to see what might lead to an improvement in eating.
The results of the assessment inform an individual plan for each child. We monitor progress during every meal by collecting behavioural information (data), and use this data to make decisions about ongoing strategies for the child.
The number of meal sessions depend on the child (e.g. nap times) but generally involve 2 to 3 meal blocks per day, over an initial 2-week period.
Some examples of interventions include:
Antecedent methods: Reducing the bite size of the food (e.g., to a pea-size) or the texture of the food, that may have reduced the effort required for eating.
Reinforcement: Providing preferred activities, foods, or a break from the meal, after eating. For example, one child initially received a break from the meal after accepting one bite of food. For another child, a preferred (nutritional) food could be chosen after eating a new food. Three children have also required reinforcement within their school meals.
Nonremoval of the spoon: In addition to the above methods, two children have required that food be present until it was accepted (or until a meal time limit was reached).
Following training, caregivers run meals with frequent support and meals are introduced to daycares or schools. Dietitians determine tube feeding reductions based on progress, usually as part of joint clinic visits.
At the end of the intervention, we visit the child at 1, 3, 6 and 12 months, to monitor progress (Follow-up)
What are the outcomes?
We look at the change in mealtime behaviours: how often the child accepted foods, swallowed foods, or displayed challenging behaviours (like pushing the plate). 10 of the 12 children achieved all their behavioural goals during ongoing family meals – eating at least 80% of foods presented across food groups (fruit, vege, protein, carb), with low levels of challenging behavior.
For 10 of 12 children, oral intake increased to allow reductions in tube feeding, and 9 children ceased tube feeding completely by the final follow-up. One child became frequently unwell and did not complete the intervention. Two children had tube feeding reductions, with one ceasing tube feeding within two years.
Based on a formal survey, we have noted some changes in stress for individual caregivers, but we have not yet seen large changes across the group. This may be because our stress survey also looks at non-feeding concerns (e.g., the stress of medical appointments or having a child with a disability).
Caregivers and health professionals provide feedback on the methods used in this research, and the benefits. Caregivers and health professionals have reported high levels of satisfaction in all areas, and some note that the home setting is key to success.
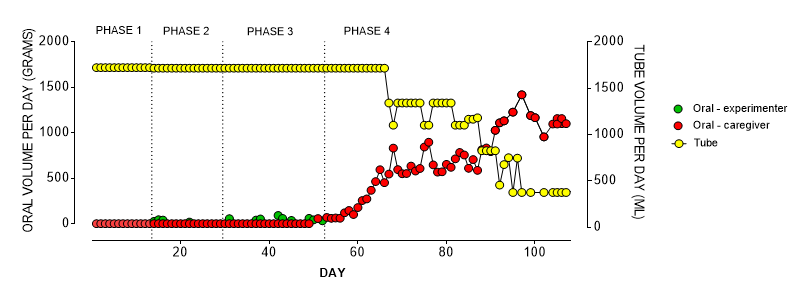
This is an example of how we tracked oral intake (in grams eaten per day) and tube intake (% nutrition that was provided via the tube)
Some things we are doing better
Given the home-based location and one psychologist, it is difficult to provide the same intensity of service that highly staffed programmes can. However, we now have postgraduate research students who provide additional supports to families during the process.
We are typically trying to start intervention when tamariki are younger and are not yet in daycare or school settings. This is helping to reduce the barriers to families that might occur when their child is older (e.g., going back to work, siblings).
Some recommendations we can make
Health services in New Zealand
Results continue to provide evidence that children with tube dependency can benefit from home-based behavioural interventions
A thorough medical evaluation, and the ongoing involvement of a mulitdiscplinary team is vital.
Pre-treatment planning with families is required to identify barriers and prepare necessary resources that could help the child reach full oral feeding (e.g., care of siblings)
As of the date of writing, many of these recommendations are in progress with the Clinical Network for Pediatric Tube feeding
Areas for future research
Future research could be improved by comparing children who are waitlisted versus children who have the intervention straight away
Working on consistent timelines and procedures, such as weeks in assessment or treatment, number of sessions per week, and health professional involvement (e.g., frequency of clinics).
Future research will also be stronger if there is more frequent health professional involvement, such as reviewing tube feeding reductions more often.
Here’s the details and link to the published study:
Sarah Taylor, Suzanne C Purdy, Bianca Jackson, Katrina Phillips, Javier Virues-Ortega, Evaluation of a Home-Based Behavioral Treatment Model for Children With Tube Dependency, Journal of Pediatric Psychology, , jsz014, https://doi.org/10.1093/jpepsy/jsz014
Are you interested in finding out more about feeding research studies? See research page here
Are you looking for help with your child’s eating? See services here